The Gut-Brain Axis
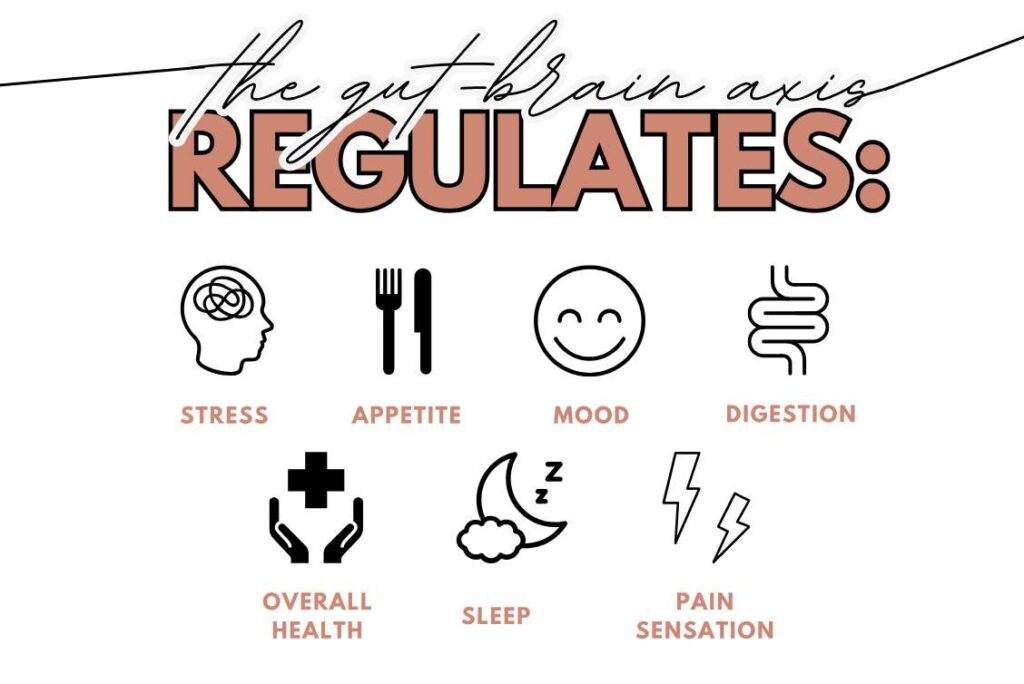
The gut-brain axis is a communication network that connects the gut and the brain, allowing them to exchange information and influence each other’s function. This communication is bidirectional, meaning that signals can travel from the gut to the brain and vice versa.
The gut-brain axis is composed of various components, including the vagus nerve, neurotransmitters, hormones, and immune cells. When you eat food, your gut sends signals to your brain that indicate whether you are full or hungry. In turn, your brain can affect the movement of food through your digestive system by sending signals that stimulate or inhibit digestive activity.
Research has shown that imbalances in the gut microbiome can affect the gut-brain axis and lead to conditions such as irritable bowel syndrome (IBS), anxiety, and depression.
By understanding and optimizing the gut-brain axis, we can promote better overall health and well-being.
The Role of Serotonin and the Gut Microbiome
Changes in gut microbes affect serotonin production and signaling, which can impact mood regulation and contribute to depressive symptoms.
The gut provides approximately 95% of total body serotonin, most of which exists in plasma. Although serotonin has intrinsic roles in the intestines and peripheral metabolism, it is capable of locally activating afferent nerve endings that are connected directly to the central nervous system. Stress and anxiety can alter the gut microbiome and lead to changes in serotonin production and signaling, which may also contribute to gastrointestinal disorders such as irritable bowel syndrome (IBS).
Overall, the relationship between serotonin and the gut-brain axis highlights the interconnectedness of different systems in the body and the importance of considering holistic approaches to health and wellness.
The Role of Cortisol and Inflammation
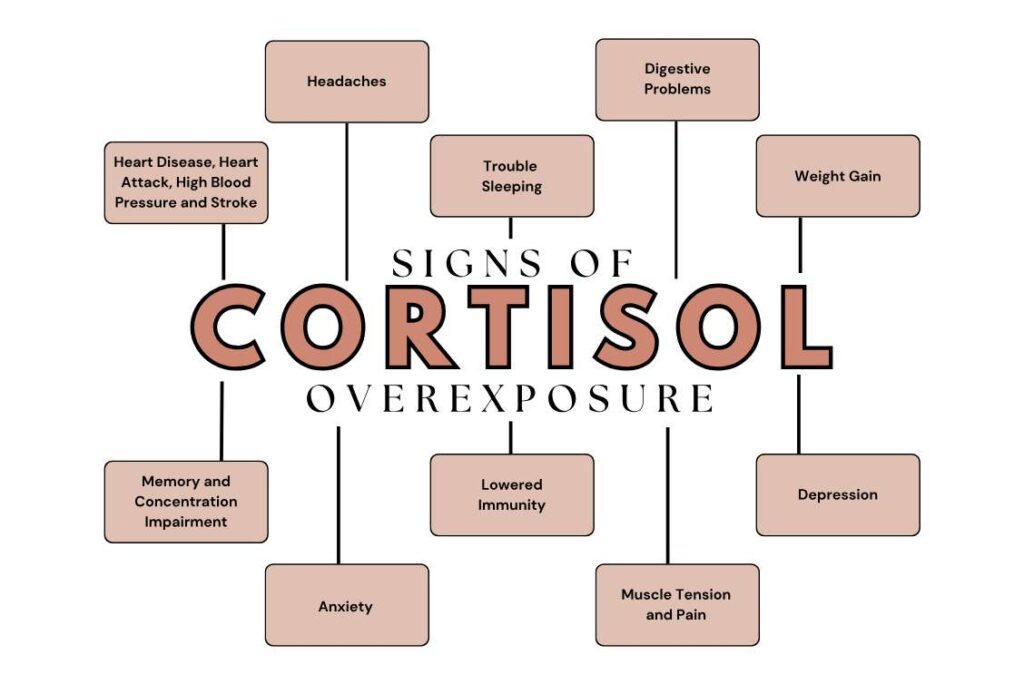
Cortisol is a hormone released by the adrenal glands in response to stress. It plays a crucial role in the body’s stress response and helps regulate various physiological processes. While cortisol is essential for short-term stress adaptation, long-term activation of the stress response system and the consequent overexposure to cortisol can disrupt almost all of your body’s processes.
Inflammation occurs when the body senses an irritation in the digestive tract – the immune system kicks in by sending extra fluids to flush out harmful bacteria or help the body heal from the perceived distress. Once stress subsides and the inflammation reduces, the intestines and bowels begin filtering correctly and the immune system stops the inflammatory process.
When stress causes cortisol levels to rise, many people experience stomach problems such as cramping or loose bowel movements. This is a direct result of the digestive system responding to increasing cortisol levels, which cause a direct decrease in the flow of blood and oxygen to your stomach. The muscles of the digestive system being affected by cortisol causes inflammation and disrupts the balance of the gut microbiome. This is why chronic stress leads to long-term digestive issues.
Improve your Mental Health by Improving your Gut Health
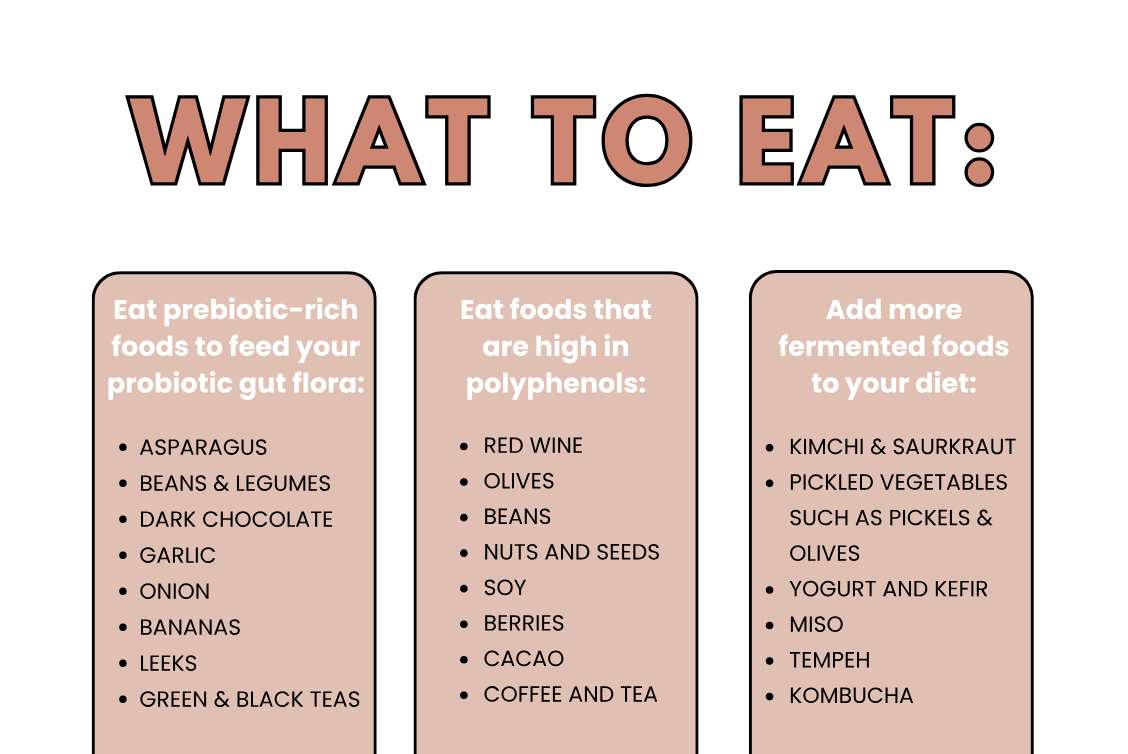
Studies show that food emulsifiers, found in processed and prepackaged foods, can cause inflammation. Maltodextrin, carrageenan, polysorbate-80, and carboxymethylcellulose are examples of common chemically processed dietary emulsifiers to look out for on ingredient labels. Since these additives are only found in packaged, processed foods, centering your diet around whole, minimally processed foods is an easy way to avoid them.
Avoid artificial sweeteners, and instead consume raw sugar in moderation. Look out for saccharin, sucralose, aspartame, acesulfame potassium, neotame, and advantame on ingredient labels of foods, beverages, and supplements.